Abstract
Introduction: The safety and clinical activity of low-dose hypomethylating agents (HMAs; parenteral decitabine or azacitdine) for patients with LR-MDS has been reported (Jabbour et al, 2017). Oral decitabine/cedazuridine (ASTX727; fixed-dose combination of 35 mg decitabine/100 mg cedazuridine) is an oral DNMTi that provides equivalent exposure to intravenous decitabine at a standard dosing (SD) regimen (20 mg/m2 days 1-5 every 28 days; Garcia-Manero et al, 2020). An effective oral HMA therapy for patients with LR-MDS that reduces the number of transfusions while avoiding the toxicity associated with both myelosuppression and parenteral administration could ease the burden of HMA administration on patients and caregivers with potential improvement of quality of life. The Phase 1 part of this study explores the optimal dosing schedule of LD oral decitabine/cedazuridine in patients with LR-MDS.
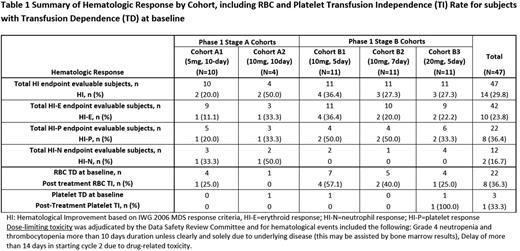
Methods: A two-part Phase 1/2 study (Phase 2 ongoing) is being conducted at US and EU medical centers in subjects with LR-MDS (IPSS low risk and Int-1). Dose selection for the ASTX727-03 Phase 1 study was divided into two phases (Stage A and Stage B). Phase 1 Stage A was designed to approximate the total dose of intravenous (IV) DEC (20 mg/m2 for 5 days) over a longer dosing period and randomized subjects to 3 Cohort regimens of 5 (Cohort A1), 10 (Cohort A2), or 15 mg (Cohort A3) DEC /100 mg CED daily for 10 days in 28-day cycles. In Phase 1 Stage B, subjects were treated with the following 3 LD oral decitabine/cedazuridine regimens of shorter duration; Cohort B1: 10 mg DEC / 100 mg CED daily for 5 days, Cohort B2: 10 mg DEC / 100 mg CED daily for 7 days, Cohort B3: 20 mg DEC / 100 mg CED daily for 5 days. Primary endpoints include determination of dose-limiting toxicity (DLT), frequency and severity of treatment-emergent adverse events (TEAEs), and the recommended Phase 2 dose (RP2D). Secondary endpoints include: pharmacodynamic (PD) activity, pharmacokinetics (PK), and clinical activity based on International Working Group (IWG) 2006 MDS response criteria and transfusion independence, Leukemia Free survival (LFS), and overall survival (OS).
Results: At the data cut-off date of June 17, 2022, 48 LR-MDS subjects were enrolled, and 47 received study treatment. Characteristics were: median age: 76 years (range 51 - 88), male: 31 (65%), and IPSS LR: 15 (31%) and Int-1: 33 (69%), respectively. The median duration of exposure is 9 cycles (range 1-34).
In Stage A, cohort A2 (10 mg, 10-day) was closed due to hematologic DLT (see Table 1) in all four treated subjects, hence cohort A3 (15 mg, 10-day) was closed prior to any subjects being randomized to that regimen. The final number of subjects treated in cohorts A1 (5 mg, 10-day), A2, and A3 were 10, 4, and 0, respectively. In Stage B, 33 subjects were randomly assigned to cohorts B1 (10 mg, 5-day), B2 (10 mg, 7-day), or B3 (20 mg, 5-day), with 11 subjects each treated with the respective dosing schedules. DLT was observed in 3 (30%), 4 (100%), 3 (27%), 7 (70%), and 7 (64%) subjects in Cohorts A1, A2, B1, B2, and B3, respectively. The DLT incidences were proportional to the dose intensity (total DEC dose per cycle) and number of days of study drug administration. All DLTs were related to neutropenia and in general regimens with higher total doses of DEC per cycle (Cohorts A2 and B3) had deeper neutrophil nadirs while regimens with longer dosing periods (7-10 days; Cohorts A1, A2, and B2) required longer to recover neutrophil counts to baseline and dose reductions and dose delays were observed more frequently than in Cohort B1. Adverse events were similar to those reported for standard dose oral decitabine/cedazuridine, with the most common grade ≥ 3 TEAEs being neutropenia (36%), anemia (28%), and febrile neutropenia (19%).
Clinical activity by dosing schedule is shown in Table 1, and bioavailability was confirmed by PK analysis. Of the 47 treated subjects, 22 subjects (47%) had reached the event of death as of the data cutoff date and median OS time was 929 days (95% CI: 526, NE). Median LFS was 690 days (95% CI: 428, 934).
Conclusions: Based on the results of the Phase 1 study, the dosing schedule of 10 mg DEC / 100 mg CED daily for 5 days, that balanced clinical efficacy with an acceptable and manageable safety profile was selected as the RP2D. This regimen will be compared to 35 mg DEC / 100 mg CED for 3 days in a 28-day cycle in the ongoing Phase 2 study.
Disclosures
Garcia-Manero:Genentech: Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; BMS: Consultancy, Honoraria, Research Funding; Acceleron Pharma: Consultancy; Gilead Sciences: Research Funding; Aprea: Honoraria; Curis: Honoraria, Research Funding; Astex: Consultancy, Honoraria, Research Funding. Sallman:BMS: Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Nemucore: Membership on an entity's Board of Directors or advisory committees; Syndax: Membership on an entity's Board of Directors or advisory committees; Kite: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Intellia: Membership on an entity's Board of Directors or advisory committees; Agios: Membership on an entity's Board of Directors or advisory committees; Shattuck Labs: Membership on an entity's Board of Directors or advisory committees; Incyte: Speakers Bureau; Magenta: Consultancy; Syntrix Pharmaceuticals: Research Funding; Aprea: Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Consultancy; Lixte: Patents & Royalties: LB-100. Al-Kali:Astex: Other: research support to institution. Berdeja:My institution, Sarah Cannon Research Institute, received consultancy payments for the following: Bluebird bio, BMS, Celgene, CRISPR Therapeutics, Janssen, Kite Pharma, Legend Biotech, SecuraBio, Takeda: Consultancy; My institution, Sarah Cannon Research Institute, receives research funds in my name for the following: 2Seventy bio, Abbvie, Acetylon, Amgen, Bluebird bio, BMS, C4 Therapeutics, CARsgen, Cartesian Therapeutics, Celgene, Celularity, CRISPR Therapeutics,: Research Funding. Griffiths:Astex Pharmaceuticals: Research Funding; BMS/Celgene: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Blueprint Medicines: Research Funding; Celldex Therapeutics: Research Funding; CTI Biopharma: Consultancy, Membership on an entity's Board of Directors or advisory committees; Genentech: Consultancy, Membership on an entity's Board of Directors or advisory committees; Medicom Worldwide: Honoraria; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Physician Educational Resource: Honoraria; Picnic Health: Honoraria; Takeda Oncology: Consultancy, Membership on an entity's Board of Directors or advisory committees; Taiho Oncology: Consultancy, Membership on an entity's Board of Directors or advisory committees; AstraZeneca: Consultancy, Membership on an entity's Board of Directors or advisory committees; Apellis: Consultancy, Membership on an entity's Board of Directors or advisory committees; Alexion: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; AAMDSIF: Honoraria. Mohan:Incyte: Research Funding; Astex: Research Funding. Sano:Astex Pharmaceuticals, Inc.: Current Employment. Oganesian:Astex Pharmaceuticals, Inc.: Current Employment. Keer:Astex Pharmaceuticals, Inc.: Current Employment. Yacoub:Stemline Therapeutics: Research Funding; Servier: Consultancy; Notable Labs: Consultancy; Gilead: Consultancy; AbbVie: Consultancy; Apellis: Consultancy; Agios: Consultancy; Acceleron Pharma: Consultancy; Novartis: Consultancy; Pfizer: Consultancy; PharmaEssentia: Consultancy; CTI Pharma: Consultancy; Incyte: Consultancy, Speakers Bureau.
OffLabel Disclosure:
This is a trial to explore optimal dosing schedule of low-dose ASTX727, including lower-risk MDS patients off-label Indication
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal